By Emma Black
The group of young men gathered under a makeshift overhang known as an “ataya base”, in downtown Freetown, Sierra Leone. The discussions (and arguments) revolve between Premier League football, politics, the price of a bag of rice, and money hustles (or the lack of). The local “ataya base” is a meeting point, like a small-town coffee shop. But, one topic that seems to be off-limits is health, especially sexually-transmitted diseases.
Twenty-five-year-old, Mohamed Kabbah, is a regular attendee among his circle of friends. He said, “Talk of health… we don’t usually… because we all know we’re sitting on a ticking time-bomb. Yes, we’re all at risk but we ignore it.”
When asked directly about sexually-transmitted infections (STIs) and the human papillomavirus (HPV), Kabbah and his mates grow silent. When pressed, the small circle of young men admit they know nothing about HPV, cancers that affect men or life choices to help prevent cancer.
Often not discussed and usually not addressed is the issue of HPV infections in men and the role of men and boys in the transmission of SDIs and specifically HPV.
Sierra Leone is blessed and cursed with a very youthful population. According to Statistics Sierra Leone, in 2019, 60% of the population was below 24-years and 41.5% of the population was below 14-years. UNICEF plots 48% of the population of around 8 million as below the age of 18. For these young people, many of whom are in the throes of puberty, life can be very challenging. These challenges put many young men and especially women at very high risk of sexually transmitted HPV.

The lack of knowledge and misinformation about sexual reproductive health is staggering. A local businessman, 45-year-old, Abdul Kargbo, admitted, “I know practically nothing about my own health. What I do know, I’ve learned just through experience. I know I don’t want to get sick.” While discussing cancer and lifestyle choices, Kargbo said, “I know we have a cancer problem in Sierra Leone but there isn’t anything we can do about it.” He added, “I don’t know anything about viruses that cause cancer or HPV… but I don’t smoke.”
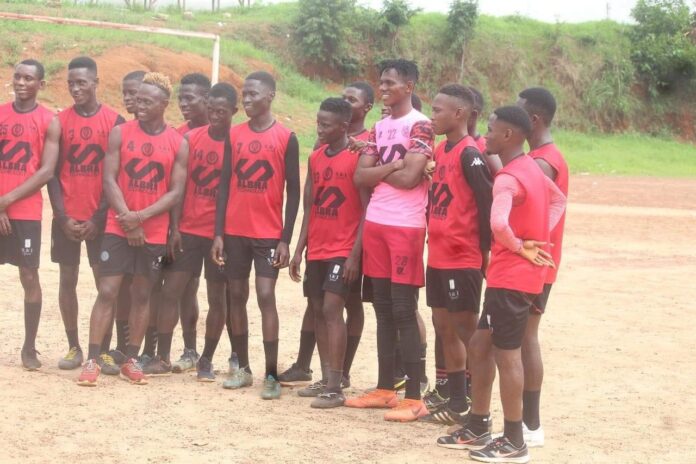
Amongst a group of teen boys, playing football on a bare patch of ground in Murray Town, 14-year-old, Peter Bangura said, “I have no idea about any virus that causes cancer. We’re not taught about that stuff in school.” Nine-year-old Abdul Karim Jalloh, reinforced their mutual lack of knowledge. He said, “I’ve never heard of that HPV virus or any kind of cancer for men.”

Moses Kanneh, 14, is about to enter junior secondary school, and is amongst a cohort of millions of other girls and boys at a similar life stage. He said, “I like science and at my school we had a lesson on health but I don’t know anything about cancer or viruses except COVID-19 and Ebola.”
A review of the National Curriculum Framework and Guidelines for Basic Education Using the Sexuality Review and Analysis Tool (SERAT), in 2020, sponsored by UNFPA, UNESCO and using International Technical Guidance on Sexuality Education, revealed, “Pupils lacked basic information about their sexual organs, healthy relationships with the opposite sex, harmful practices and an understanding of gender.” The study also found, “Teachers (40% of whom were untrained and volunteer) were using their discretion by teaching about violence and consent and bodily integrity, albeit with a fear-based approach. It was also apparent that lessons often contained messaging that perpetuated gender unequal norms and attitudes.”
The 2020 assessment of curriculum found, “Between 12-15 years there was no teaching on sexuality and sexual behaviour and teaching on sexual and reproductive health was “present to some extent.” The same curriculum assessment on primary school curriculum, between 5-8 years, found there was no teaching on Understanding Gender, Violence and Staying Safe, Skills for Health, Human Body and Development, Sexuality and Sexual Behaviour and Sexual and Reproductive Health.
In 2022, the Ministry of Basic and Secondary School Education (MBSSE) introduced a new curriculum, which should help improve reading levels and the quality of sexual and reproductive health education for children.
The US Center for Disease Control and Prevention (CDC) reports, “Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States among 15 to 50-year-olds. The CDC notes, “2 in 5 (40%) people will have HPV and approximately 85% of Americans will have some form of human papillomavirus (HPV) in their system during their lifetime. There are no HPV statistics for Sierra Leone yet.
Most sexually active adults have already been exposed to HPV, which is spread by having vaginal, anal, or oral sex with someone who has the virus. It also spreads through close skin-to-skin touching during intimate activities. HPV can spread even when a person with the infection has no signs or symptoms.
Unfortunately, there is no test for a man to check his overall HPV status. Many times, men only become aware of the infection after a secondary problem develops such as genital warts. However, most men are asymptomatic, meaning they will never develop symptoms. This makes the virus even more dangerous and dramatically increases the risk of transmission of HPV, especially if multiple partners are involved.
The CDC and the WHO warn, “The infection usually goes away by itself. But, if HPV does not go away, it can cause genital warts or certain kinds of cancer.” An Australian medical report notes, “Men with HPV infection are more than twice as likely to develop prostate cancer than uninfected males, and cancerous prostate lesions are more likely to harbour highly pathogenic types of the virus when compared to benign lesions.” In Australia, HPV is the likely cause in approximately 63%, 89% and 72% of penile, anus and throat cancer cases. What’s important is that the HPV vaccine is safe and extremely effective against HPV infection and related lesions in males (and females) for years. Australia leads the world with vaccination against HPV, having the first national vaccination program (commencing for females in 2007 and expanding to cover males in 2013) and current coverage of more than 80% of 15-year-old females and over 75% of 15-year-old males. HPV vaccination is also very important for males.
Health and Sanitation Minister, Dr Austin Demby, noted, “Our HPV vaccination initiative is part of a broader vision for women and girls… and society.” He said, “If you don’t have enough vaccines for everyone, you prioritize, so right now the most vulnerable are the girls and that‘s where we’re prioritizing. I think if we’re able to demonstrate the kind of coverage and opportunities for us to expand this I think we would love to immunize all boys as well. We’re not doubling the effort because we’re already there; the structure is there already; the systems are there and I really love this idea of vaccinating boys as well.”
According to the WHO, HPV symptoms can appear on a penis, scrotum, anus, mouth, or throat. Genital warts usually appear as a small bump or group of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower. If warts or growths appear, the WHO and other healthcare advisors say people should immediately visit their healthcare provider.
HPV itself isn’t cancer but it can cause changes in the body that lead to cancer. HPV infections can cause certain kinds of cancer to grow. These include: cervical cancer in women, penile cancer in men, anal cancer in both women and men, cancer in the back of the throat, including the base of the tongue and tonsils. All of these cancers come from HPV infections that did not go away.
There are basically just two steps to take to lower the risk of getting HPV and diseases from HPV. 1) Vaccination. The HPV vaccine is safe and effective. It can protect men against warts and certain cancers caused by HPV. The HPV vaccination is recommended for all preteens (including boys and girls) at age 11 or 12-years (or can start at age 9 years) and everyone under 25-years. 2) Proper use of condoms. This can lower the risk of getting all STIs, including HPV. However, HPV can infect areas the condom does not cover. So, condoms may not offer full protection against getting HPV.
“We are in the era where no one should suffer or die from diseases that are preventable with the use of vaccines. And, we will make these lifesaving services accessible to safeguard the health of women and girls,” said Dr Steven Velabo Shongwe, WHO Representative in Sierra Leone.
In many cases, men are not aware of the infection and therefore, unknowingly pass it through sexual intercourse. The odds of spreading it increase with casual sex practices or multiple sex partners.
In 2020, there were 4,708 new cancer cases detected among men and women. Breast cancer accounted for 20.9% or 985 cases. Cervical or cervix uteri cases accounted for 10.7% or 504 cases. Out of the 4,708 cancer cases, there were 1,836 men who were diagnosed with cancer. There were 2,189 “other” cancers recorded including 222 colorectum cases, 407 liver cancer cases, and 407 prostate cancer diagnosis. WHO figures indicate that if a person is diagnosed with cancer in Sierra Leone they have a 73% chance of dying… or a 27% chance of survival.
Over a heated discussion about the state of Sierra Leone’s healthcare system, 26-year-old Musa Paul Feika and Rangen Conteh, 35, admitted to knowing very little about cancers that affect men. Conteh said he had never heard about HPV or any kind of vaccine that might prevent cancer.
The daily gathering of groups of young men is evidence of the lack of employment opportunities in the country. In 2022, the UNDP noted 70% of youths in Sierra Leone are currently underemployed or unemployed, and 50% illiterate and unskilled. According to a report released in November 2021, by UNICEF and the Ministry of Basic and Senior Secondary Education (MBSSE), more than half of 15-year-olds and above (57%) were illiterate and half of those leaving primary school were unable to read or write.
Sierra Leone continues to be ranked among the bottom countries of the world in the UNDP Human Development Index. Shockingly, 81% of its population lives in poverty and 59.2% living in extreme poverty living on less than $1.25 per day and around (55%) are estimated to be food insecure according to a UNDP report in 2020.
In 2022, the Advocacy Network for Community Development (ANCD) in Sierra Leone, conducted a survey of 180 recent university graduates across six university campuses. Almost 12-months after graduation, 7 out of every 10 graduates interviewed said they have not found a job. The civil society organization noted, “Unemployment rate for new graduates in Sierra Leone hit a record high of 72%, in 2022.
The National Youth Commission, with UNDP, noted in 2020, “Young people face a high level of inactivity, unemployment and under-privileged working conditions characterized by low wages and long working hours. Poor quality of education, poor health facilities, spread of HIV/AIDS, the ever-increasing teenage pregnancy and drug abuse are also among the challenges that affect the quality of young people’s life. More than 60% of youth in Sierra Leone are either unemployed or underemployed and more than 50% of the country’s youth are believed to be either illiterate and/or unskilled.”
At the “ataya” base, Ibrahim Sankoh, 23, said, “We cannot get sick. If we do, we have to spend money we don’t have. We can go to the hospital but the system is bad… and we’ll end up dying from whatever… we don’t know.” The healthcare system is rapidly improving but in 2018, the UNFPA issued their Assessment of Adolescent and Young People Friendly Health Services. The UNFPA noted, “Only 17% of the health facilities surveyed had all contraceptives; 50% had HIV posters and far fewer (16.7%) had posters on STIs. Most centres (86.7%) had no brochures regarding SRH.”
The safe, effective HPV vaccine has been available in most wealthier countries since the 2000s. Gavi, the Vaccine Alliance, and its partners are now working to ensure the vaccine is available to girls across the world: Sierra Leone is the 19th African country to introduce the vaccine.
The Minister of Health, Dr Demby, noted, “The science is really great and that’s the other thing that will drive this. There’s no longer a question that the HPV causes cervical cancer.” There is no longer a question that HPV also causes cancers in men.
Over a two-week period in October 2022, Ministry of Health workers and community mobilizers were involved in a HPV vaccination campaign, sponsored by Gavi, the Vaccine Alliance, UNICEF and WHO, that inoculated more than 182,000 girls between 10 and 14-years-old.
A Gavi spokesperson said, “As part of our partnership and collaboration with Sierra Leone lasting over two decades, Gavi, the Vaccine Alliance in 2022 supplied 193,900 doses for the initial introduction of the vaccine into routine immunization. The cost of the doses was estimated at approximately $900,000 USD with an additional 23,500 doses supplied through country co-financing avenues. Gavi has also provided $950,000 in delivery support, for example and the installation of solar refrigerators and training for 1,500 healthcare workers.
Following the introduction, Gavi is now supporting the HPV doses that will be needed for routine immunization of girls every year. Based on the current forecast and projections, support for the next five years is estimated at about 125,000 doses every year with Gavi’s contribution estimated at about $570,000 USD annually towards the cost of the vaccines. This is part of an estimated $20 million for additional operational and technical funding support earmarked for routine immunization activities including HPV over the next five years.
“The campaign is a first step towards protecting girls in Sierra Leone from cervical cancer and providing them with a better chance of living longer, healthier lives and reaching their full potential,” said Thabani Maphosa, the Managing Director of Country Programmes at Gavi, the Vaccine Alliance. “Historically, HPV coverage worldwide, but especially in lower-income countries where the cancer burden is highest, was already too low.”
In the medical journal, Frontiers in Cellular and Infection Microbiology, in December 2022, the article, Prevention and Treatment of Human Papillomavirus in Men Benefits Both Men and Women, highlighted, “Men should be vaccinated against HPV (this is especially true for adolescents). Nevertheless, barriers still exist to achieving prevalent HPV vaccination in men, including a lack of knowledge regarding HPV, prejudices against the vaccine, various sociodemographic and religious factors, fear of side effects, and concerns about cost.”
In Sierra Leone, it is crucial to build knowledge regarding HPV-related diseases so that more people, girls and boys, get vaccinated. At the same time, the healthcare system should make routine HPV vaccines more accessible. HPV-specific treatment and preventive efforts should not only be targeted to women, but also towards men and boys.
“This reporting was supported by the International Women’s Media Foundation’s Global Health Reporting Initiative: Vaccines and Immunization in the Caribbean, in partnership with Sabin Vaccine Institute.”